Achieve Optimal Outcomes and Cost Savings with Gray Matter Analytics Solutions
Elevate quality of care & facilitate health equity
View performance against financial, utilization and quality measures across multiple contacts to engage providers, efficiently manage service to members and support delivery of the highest quality care possible. Monitor and measure quality of care, assess program and intervention effectiveness, and identify need for improved health equity and population health.
Reduce avoidable spend
Manage costs and maximize revenue by identifying high-risk populations, tracking utilization patterns and allocating resources where they can have the greatest impact.
Monitor care coordination
Ensure members and populations receive directed, efficient care toward better health outcomes at lower costs. Track member interactions with providers, identify gaps in care and highlight outreach opportunities through analytic insights.
Evaluate value-based care models
Assess CMS and commercial models for their success in maintaining or improving quality of care at reduced or static cost. Create payment models and incentives to enhance primary care services, prevention and disease management.
Manage compliance with standards
Mitigate potential risks and stay compliant with regulations and reporting requirements, including Medicare Advantage and Medicaid cost measures.
Maximize your revenue potential with contract-level insights — uncover hidden value, prioritize revenue-generating opportunities and mitigate potential risks.
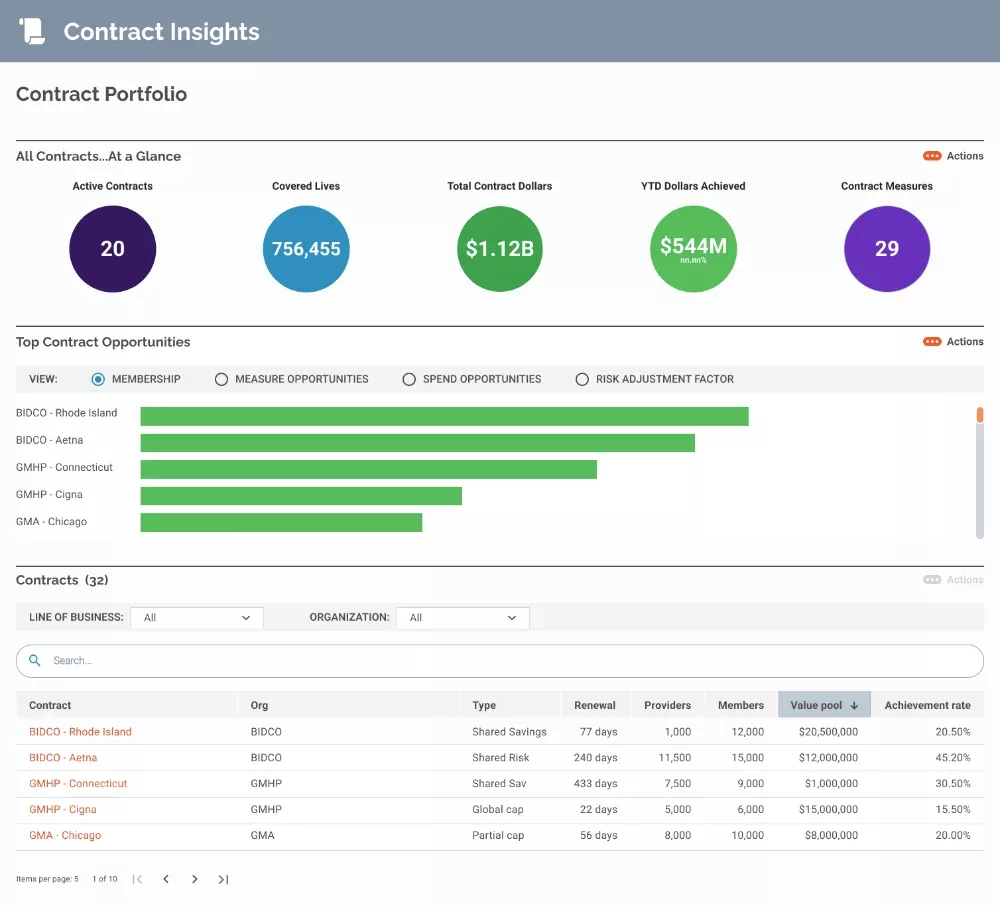
- Contract performance management: Analyze the cost impact of current programs and forecast trends in measure performance and quality outcomes to achieve goals across total spend and drive higher engagement.
- Contract data integration: Use integrated claims, utilization and related healthcare data to identify and eliminate low-value services and emphasize those that have a greater impact on quality goals and health outcomes.
- Configurable contract visualization: Customize dashboards for easy views of contract performance, trends and improvement opportunities at individual and aggregate levels.
Monitor provider progress against goals, stay on top of HEDIS measures and drive improved member outcomes.
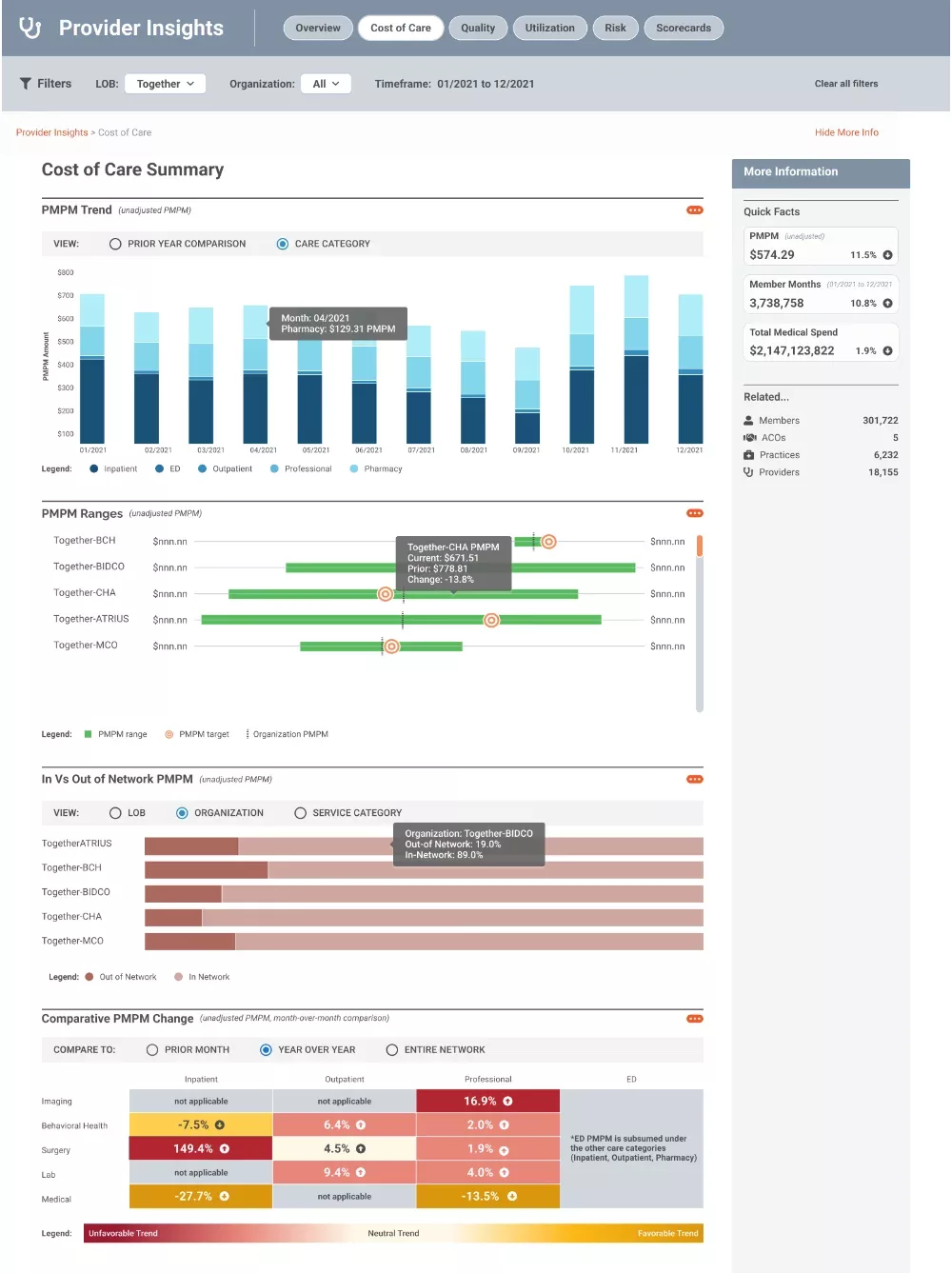
- Provider performance assessment: Monitor quality and utilization trends to determine whether members are receiving appropriate care.
- Provider performance monitoring: Identify drivers of adverse trends and outliers, and partner with providers to develop improvement programs.
- Category cost comparison: See year-over-year changes and trends toward or away from goals at the adjusted and unadjusted per member per month rate and for overall medical spend.
Prevent and manage preventable health risks and data-driven insights — target high-risk populations, understand contributing factors and prioritize interventions.
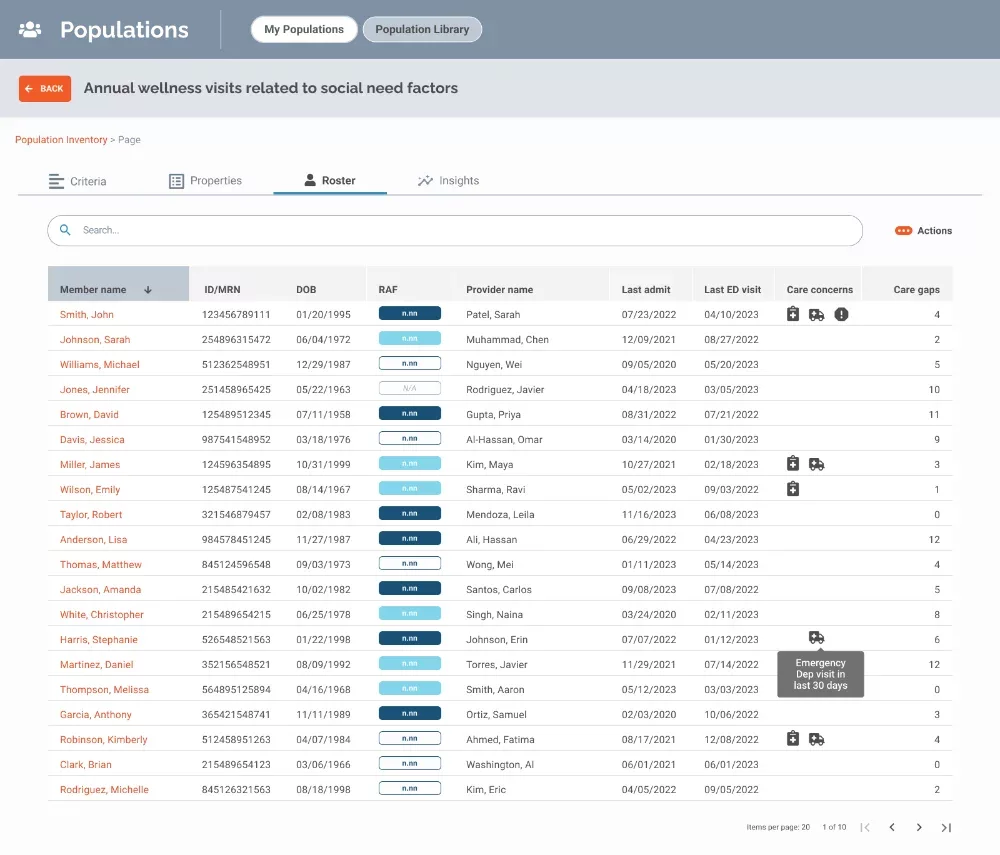
- Member screening and risk stratification: Identify patients for targeted interventions by efficiently analyzing data based on measures, cost, demographics and practice/provider attribution.
- Custom communication cohorts: Prioritize high-value patient subgroups for education and management.
- Coordinated member engagement reports: Automate ongoing measure adherence monitoring at the member or cohort level.
Trusted by:




I’ve looked at several different tools, and CoreTechs® is the only one that brings in social determinants of health, contract management and population insights — everything we need to be able to manage contract and follow our patients to see where they are slipping through the cracks.
Gray Matter showed us how we could reduce manual referrals and accelerate care for patients with machine learning that identifies patients who require a referral based on clinical conditions and eligibility information.
Based on the reputation of the management team at Gray Matter Analytics and their ability to demonstrate their understanding of physician performance/value-based care, we decided to become their first CoreTechs® customer. The proof of concept is continuing, and we have very high expectations on the results.
CoreTechs® brought to the surface chronic conditions like diabetes that we had not coded. From that, we learned how to capture and document risk-adjusted factors for shared savings contracts and patient enrollment in disease management programs.
We were at a loss for why our members were seeing providers outside of our network. Gray Matter gave us the analytic tools to understand who would seek an external specialist, when and why. We learned the best points along the care continuum to intervene and even the dollars at risk for each member’s out-of-network choice.
Gray Matter Analytics developed models to help us predict members at risk of postpartum depression so we could proactively offer behavioral health services and take better care of our moms and their families while reducing costs.
Data-driven insights from CoreTechs® guided physician education, code capture, patient outreach and pre-visit planning to help us meet the quality, care and cost expectations of the Medicare Shared Savings Program.
Our team was stretched thin. Gray Matter became our advanced analytics partner and helped us with important work with analytical models and capabilities in CoreTechs® that would have taken years for us to develop on our own.
A lot of times there’s a disconnect between the provider and the payor. With Gray Matter Analytics, we’re looking at the same data.
